What’s this got to do with brain tumours?
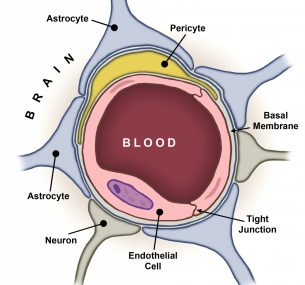
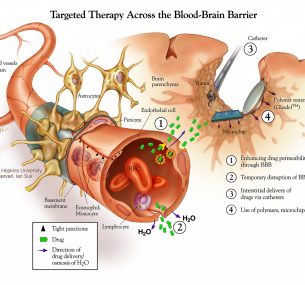
The blood-brain barrier (BBB) protects our brains from harm. But its success is also its undoing when it comes to treating neurological diseases, including brain tumours. The strict border control of the BBB restricts entry into the brain of many small-molecule drugs and nearly all large molecule drugs that have been developed to treat brain disorders. In brain tumours alone, this is a huge problem. Worldwide, around 256,000 brain and CNS tumours are diagnosed per year – that’s 700 every day. And incidence is rising, mainly due to an ageing population coupled with a lack of progress in treatment. In the UK, since the early 1990s, incidence rates have increased by around a third (34%). Add to this the fact that 30-40% of all cancers metastasise to the brain, and that bypassing the BBB is key to the effective treatment of many other neurological diseases (including Parkinson’s Disease, stroke, Alzheimer’s Disease and epilepsy), you realise that the implications of the BBB challenge are staggering. It is estimated that more than 20 million patients worldwide currently suffer from CNS-related disorders that would benefit from better transport of drugs across the BBB! It is vital that we find ways to deliver effective concentrations of drugs into the brain. This is why, in February 2016, Children with Cancer UK ran a workshop dedicated to this topic and subsequently funded the set-up of a new international initiative – the Children’s Brain Tumour Drug Delivery Consortium:
www.cbtddc.org Launched in March 2017, this initiative aims to:
(1) raise awareness of the challenge of drug delivery in childhood brain tumours and other brain diseases; and (2) initiate and strengthen research collaborations to accelerate the development and translation of drug delivery systems that target brain diseases.