I am originally from Tucuman a small town in the north of Argentina. After my PhD, I moved to the UK to further progress my scientific career. In 2009, I joined the group of Professor Gerry Melino at the MRC toxicology Unit in Leicester, as a postdoctoral fellow. The group’s main research focus is to understand the role of a family of genes, the p53-family, in the formation of tumours. In 2014, I won a prestigious fellowship from
Children with Cancer UK to work on
medulloblastoma, a rare aggressive paediatric
brain tumour and a major cause of mortality in children. We all know someone who has suffered from cancer and its’ effects. My dad has been battling colon cancer for many years now. My uncle has been struggling with a metastatic prostate cancer for two and a half years. I can empathise with the physical and emotional pain that these children and families are going through. Either way, cancer touches our lives invariably. We all hope for the development of new and more effective treatments that are accessible to all. Rare diseases are often underfunded, so the work of the few research groups that dedicate themselves to these becomes essential for finding new treatments and bringing hope to the affected kids and their families.
My work on understanding medulloblastoma
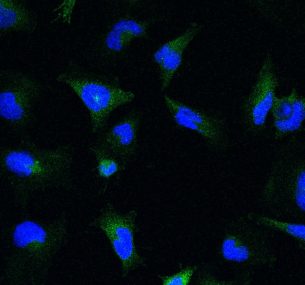
I currently work on medulloblastoma, a paediatric brain tumour and a major cause of mortality in children. These tumours are malignant and patients have to undergo aggressive treatments leaving survivors with severe side effects. Hence, more targeted and less toxic therapies are vitally needed to improve the quality of life of survivors. My work focuses on understanding the chemical reactions that allow tumours to stay alive, a process called “metabolism”. It aims at understanding how the metabolism of medulloblastoma is regulated and whether and how these tumours could be starved of essential components of their diet to strengthen the effect of
chemotherapy given to these patients. You may have heard about calorie restriction and ketogenic diets in the news. As early as 500 BC, fasting was used as an effective treatment for many medical conditions. Data from experimental and epidemiological studies indicate that obesity due to excessive energy intake and minimal physical activity increase the risk of developing cancer. In contrast, some studies suggest that calorie restriction may have several health benefits for humans like reducing the risk of developing cancer.