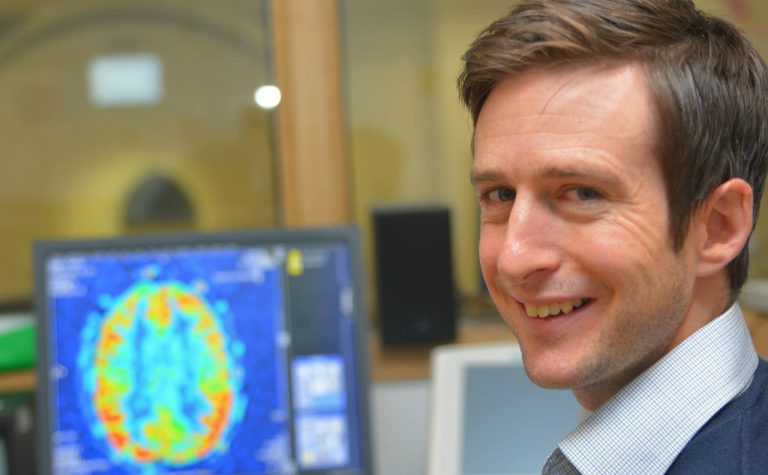
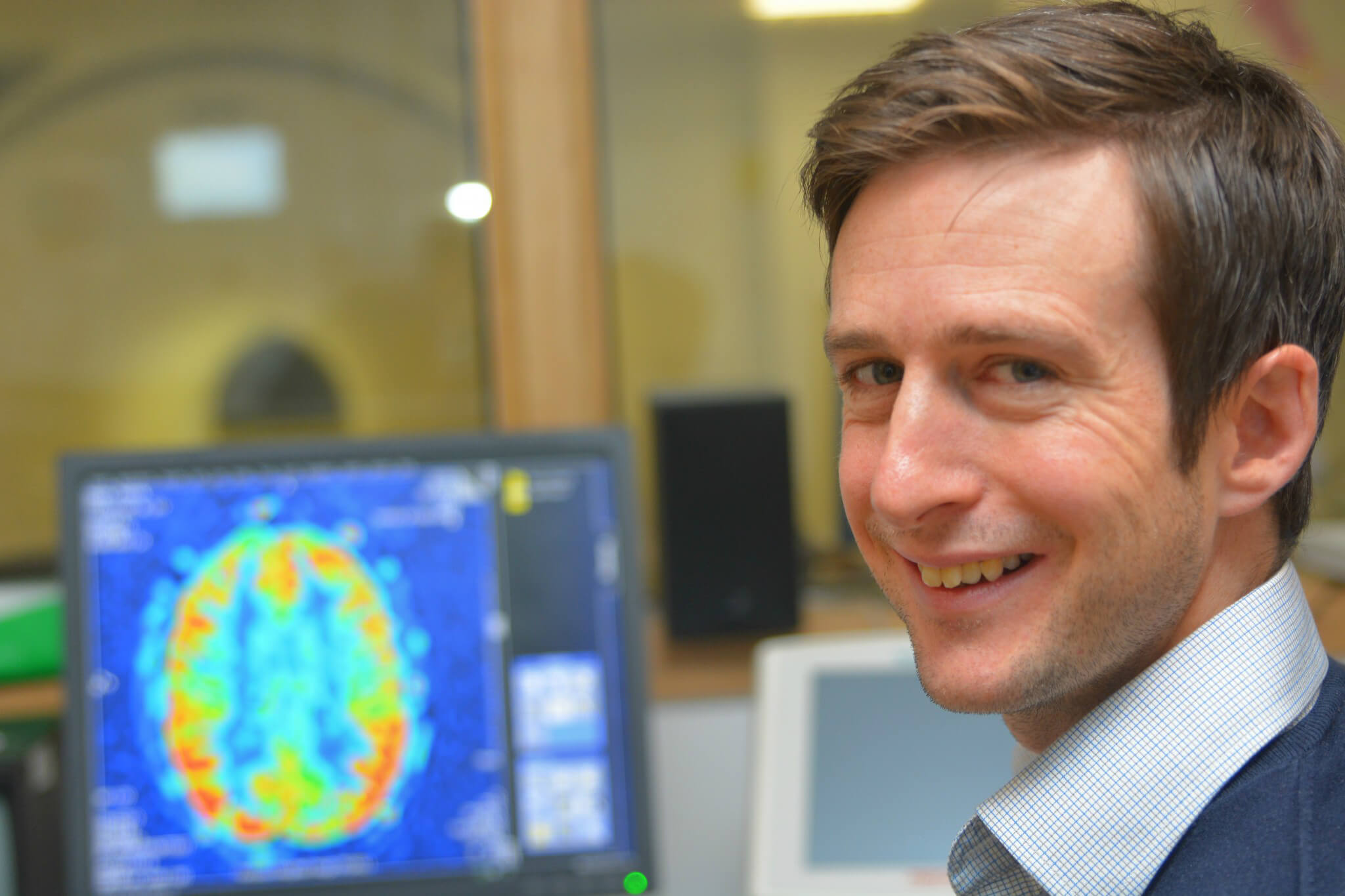
MRI scans are essential to help us diagnose brain cancers. But current techniques can’t always give us the precise information we need about what type or subtype a tumour is, its malignancy, and how far it has spread. Developing new techniques will help us learn more about a brain tumour before we operate.
This Fellowship is funding research into new scanning techniques to help us identify sub-types of brain cancer and give us more information about how to treat them.
Thank you
This research project on new MRI techniques has been successfully completed. Your donations allow us to fund ground-breaking research that can improve treatments given to children with cancer. Thank you. Your help allows us to continue to find ways to drive up the chances of survival for children with cancer and reduce the toxic side effects that can affect the rest of their lives.