Making immunotherapy better for children with acute lymphoblastic leukaemia
29 September 2025

Chemotherapy and targeted drugs will successfully treat almost 9 out of 10 children with acute lymphoblastic leukaemia (ALL), the most common type of blood cancer in under-25s.
Still, in some rare cases – among some of the youngest children – high-risk ALL can adapt to resist standard treatments. That’s why specialised ones like immunotherapy are so important.
Thanks to immunotherapy, doctors have another option when more traditional ALL drugs stop working. Now, they can train patients’ own immune cells to find and destroy their cancer.
CAR T-cell therapy and beyond
That’s one way to describe a type of immunotherapy called CAR T-cell therapy. It’s one of the world’s most advanced cancer treatments, and it’s now helping children with what were once incurable leukaemias grow up cancer free. But using it is complicated.
CAR T-cell therapy works with white blood cells called T cells, which play a crucial role in protecting our bodies from threats. Because each of us has our own unique T cells, doctors have to take a very personalised approach to turn them into a treatment.
First, they have to extract T cells from the person they’re treating. Then they need to send these cells off to the lab, where scientists equip them with special cancer detecting sensors called ‘chimeric antigen receptors’ (CARs), which are tuned to identify specific markers on leukaemia cells. After that, the T cells need to be reintroduced to the patient’s body, where they can start targeting the cancer.
All those steps make CAR T-cell therapy a very delicate procedure. Unfortunately, its complexities can sometimes lead to problems.
That’s why Professor Anindita (Andi) Roy and Professor Anastasios (Tassos) Karadimitris have spent the last four years working on an alternative. They’ve developed a way of putting cancer-detecting CARs on different immune cells – ones that can be taken from healthy donors and stored until young leukaemia patients need them.
It’s a much more accessible approach, and the team’s latest research paper has shown that it could also be more effective.
Where the clinic meets the lab
We funded this project with Children with Cancer. It started with another collaboration at the University of Oxford, between Roy’s team and Professor Tom Milne. Together, they discovered new markers on certain types of hard-to-treat ALL cells – markers we can target with CARs.
They could have used this discovery to make a new CAR T-cell, but Roy’s a clinician as well as a researcher; she works at Great Ormond Street Hospital, and she knows what using CAR T-cell therapy is like in practice.
“I’ve seen how difficult it can be to treat little babies with CAR T-cell therapy,” Roy says.
Since CAR T-cell therapy is only available after other treatments have stopped working, doctors need to collect T cells from young patients who have already gone through chemotherapy. But that damages healthy T cells as well as cancerous ALL cells, and sometimes there aren’t enough T cells left for the treatment to work. It’s a catch-22: once we know a patient needs CAR T-cell therapy, it’s less likely we can use it.
That’s just the first problem. Engineering T cells with CARs takes time, so patients with aggressive leukaemia may need a bridging treatment to keep the cancer under control while they wait. Then they need another treatment to prepare their body for the new cells. Overall, the process can take weeks, especially if patients are unwell.
“We’ve seen it happen as clinicians – you’re losing that window of opportunity,” says Roy. “And then, if the production process fails, the patient can be left with nothing.”
An ’off-the-shelf’ alternative: invariant NKT cells
So, Roy wanted to find another immunotherapy option for patients with high-risk leukaemia.
That’s where Karadimitris comes in. He was one of Roy’s mentors while she was doing her PhD at Imperial College London – and he’s a CAR specialist.
“I’m not an expert in immunotherapy,” explains Roy. “I study the biology of leukaemia, which is more about identifying the target, but to engineer the actual product we needed Tassos’s lab.”
The product she’s talking about is a special subtype of T cells called invariant natural killer T cells (iNKT cells).
The name ’invariant’ reflects the fact that everyone’s iNKT cells are the same. Unlike standard T cells, they don’t patrol our bodies looking for things they don’t recognise, so a cancer patient could receive donated iNKT cells without any issues. They’re the perfect candidate to develop a more universally deployable CAR treatment.
“I’m lucky,” says Roy. “Tassos runs one of very few labs who develop this very novel type of therapy.”
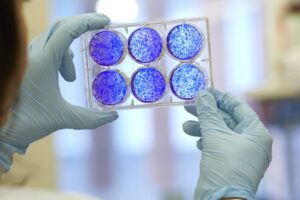
Karadimitris’ lab engineered iNKT cells with a CAR that allowed them to recognise and target two markers linked to Milne and Roy’s discovery. Then, the team at Imperial and Oxford rigorously tested how the new therapy worked using a new lab model of leukaemia and cells from ALL patients.
Double benefit
Those tests confirmed that CAR iNKT cells target cancer cells in the same way as CAR T-cells, and that they don’t have a long-term adverse effect on other healthy blood cells.
Excitingly, this means that donated iNKT cells could be used to create an ‘off-the-shelf’ immunotherapy suitable for more young patients at more points in their treatment. In other words, iNKT cells could make CAR technology as accessible as any other drug – ready to go whenever patients need it.
On top of that, Roy and Karadimitris also found that their CAR iNKT cells cleared ALL better than conventional CAR T-cells, including in traditionally difficult-to-treat sites around the brain, bone marrow, and spleen. One of the key causes of relapse from high-risk ALL is cancer cells lingering around the brain, so the findings suggest CAR iNKT therapy could keep children cancer-free for longer.
“Often in science you think something will work, and then it doesn’t,” says Karadimitris. “It very rarely happens that you deliver exactly what you hoped to achieve at the end of a four-year project, and the fact that it worked so much better than current treatment options makes it very exciting.”
We share that excitement. And now the lab work is done, it’s time to see if the new treatment can make a difference for patients.
The Cancer Research UK – Children with Cancer UK Innovation Awards
This project was funded through an Innovation Award from Cancer Research UK and Children with Cancer UK.
Gavin Maggs, CEO of Children with Cancer UK, said:
This project is a great example of how collaboration can drive forward new approaches that are not only more effective, but also more accessible for children with the most aggressive forms of leukaemia.
We’re proud to have supported this innovative research alongside Cancer Research UK. Collaboration like this, between not only funders but also universities, is essential if we’re to close the gaps in research and give every child the best possible chance. This work brings us a step closer to more personalised, kinder therapies designed specifically with children in mind.
(Originally written by Cancer Research UK, a co-funder of the research project)
About Children with Cancer UK:
Children with Cancer UK is the leading children’s cancer charity in the UK. Our vision is a world where every child and young person survives their cancer diagnosis. Our mission is to improve survival rates and the quality of survival in young patients, and to find ways to prevent cancer in the future. We are dedicated to raising and investing funds into vital research that helps us understand childhood cancers and improves treatments. We support families as they navigate treatment and life beyond cancer. What began as a small memorial charity in 1988, has evolved into a leading childhood cancer charity raising more than £300 million and investing in over 300 pioneering research projects.
Press enquiries:
For all press enquiries, please email [email protected] or call 0800 222 9000 and ask for the media team.
Other stories
We have lots of information to help you learn more about childhood cancer. From specific cancer types, to treatments and causes.