Development of natural killer cell immunotherapy for paediatric rhabdomyosarcoma
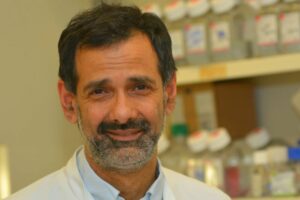
Dr Matthew Blunt aims to create and test immunotherapy treatments for rhabdomyosarcoma that are safer and more effective than chemotherapy.

Project Details
- Creating innovative new treatments for childhood rhabdomyosarcoma by harnessing the body’s natural defence system
- Lead Researcher
- Dr Matthew Blunt
- Research Centre
- University of Southampton
- City & Institution Postcode
- Southampton, SO17 1BJ
- Start Date
- 01/02/2026
- Project Duration
- 36 months
- Grant Amount
- £316,964.66
Overview
Rhabdomyosarcoma (RMS) is a soft tissue cancer that mostly affects children. Current treatments can have serious long term side effects and are not successful at treating high-risk rhabdomyosarcoma (especially when the cancer has regrown or spread around the body).
Rhabdomyosarcoma is especially good at avoiding the body’s first line of defence against cancer – the immune system. It can hide from immune cells or even switch them off. Treatments meant to reactivate the immune system work well for other cancers, but haven’t worked well for rhabdomyosarcoma. Parents and families stress the need for kinder and more effective treatments.
About the project
Dr Matthew Blunt’s team at the University of Southampton want to investigate a safer type of immunotherapy called CAR-NK cell therapy. It bolsters the body’s ability to fight cancer by attaching chimeric antigen receptors (CAR), which can bind to cancer cells, to natural killer (NK) immune cells. The resulting CAR-NK cells have the ability to ‘see’ the previously invisible cancer cells and kill them.
The researchers will investigate rhabdomyosarcoma samples to see why normal NK cells aren’t able to effectively fight the cancer. Using their findings, they will design two new treatment approaches to:
- Activate NK cells that are already present in these children to destroy their cancer cells.
- Generate billions of NK cells from healthy adult donors that can rapidly destroy cancer cells once given to patients.
These treatments will be tested in the laboratory using cutting‑edge 3D models of rhabdomyosarcoma grown from real patient tumour cells.
What difference will this project make?
This project has been developed with input from patients and families, who emphasise the need for new approaches to lessen the physical and psychological damage to children undergoing treatment for rhabdomyosarcoma. NK cells have shown excellent safety in patients and have induced complete remissions in patients for other types of cancer.
Because of this, Dr Blunt hopes that this work will lead to new treatments that can rapidly be adapted for a clinical trial. Therefore, this project has strong potential to benefit children with cancer by providing safer and more effective treatments.
Other stories
We have lots of information to help you learn more about childhood cancer. From specific cancer types, to treatments and causes.