Hodgkin lymphoma
Hodgkin lymphoma accounts for around 44% of all lymphomas diagnosed in children in the UK (1). Although the cure rate is high, it’s easily mistaken for other diseases, like glandular fever. Finding a simple way to diagnose it earlier would help children avoid unnecessary illness, and maybe mean less intensive treatment. Hodgkin lymphoma is distinguished from other types of lymphoma by the type of cancer cell formed – the Reed-Sternberg cell – which is not found in any other blood cancer.
Proteins secreted by tumour cells can be detected in the blood. We’re testing whether this can be used in the early detection of tumours.
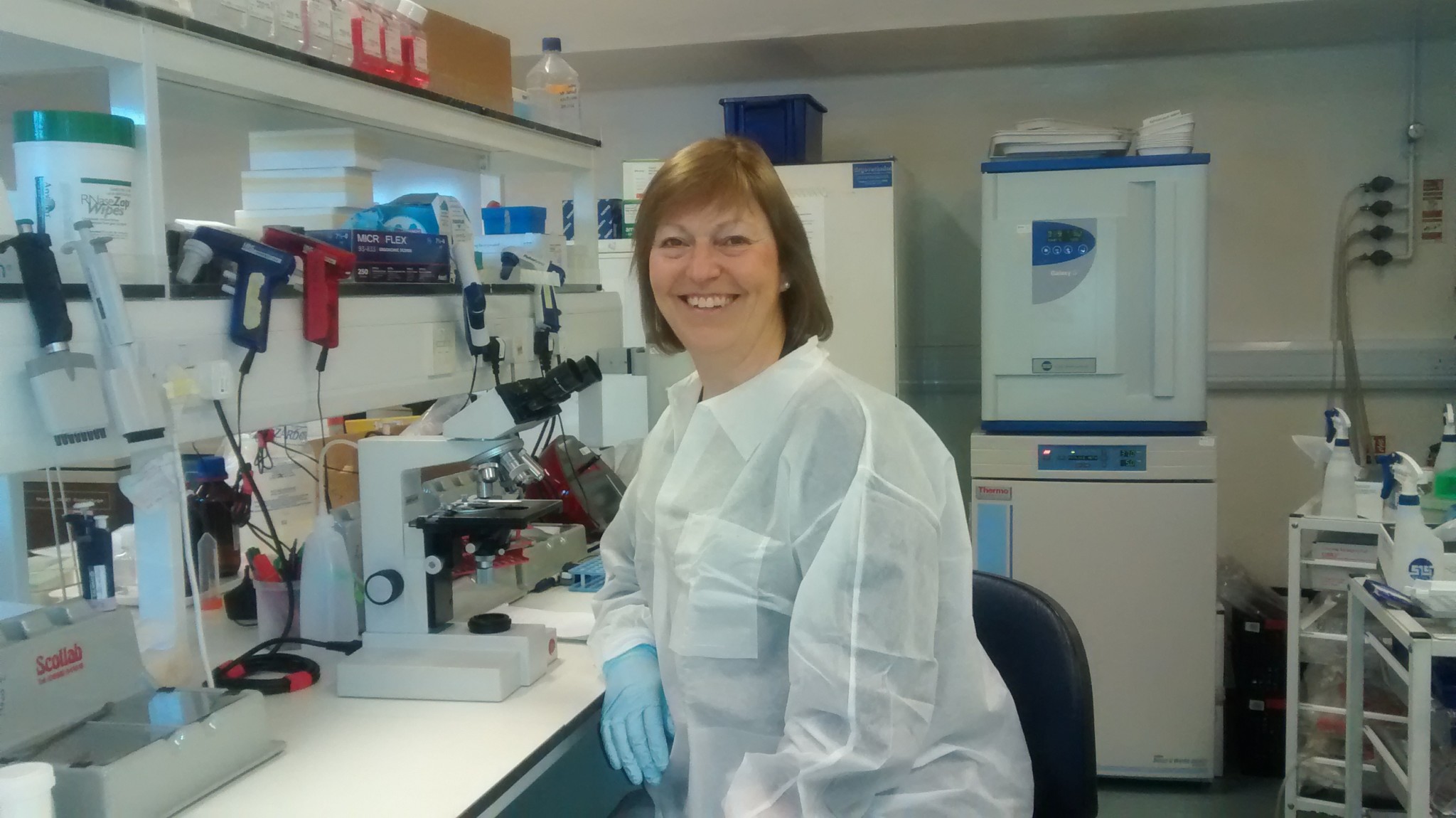
Prof Ruth Jarrett, University of Glasgow.
Professor Ruth Jarrett, who we’re funding to find a simple way to diagnose Hodgkin lymphoma earlier in children and avoid unnecessary illness.