What is Hodgkin lymphoma?
Lymphomas start in the lymphatic system, the network of vessels that runs throughout the body carrying fluid containing white blood and other important immune system cells. Lymph nodes respond to infections by releasing white blood cells called lymphoid cells into the blood stream to fight it off.
When someone has lymphoma, lots of abnormal lymphoid or lymphoma cells are produced within a particular lymph node.
These are the same cells that become cancerous in people who have leukaemia, another form of blood cancer. The difference is that leukaemia develops in the bone marrow and affects normal blood cell production. Lymphoma, on the other hand, develops in the lymphatic system and does not affect normal blood cell production.
In patients with lymphoma the cancer cells cluster in the lymph nodes and form tumours. These cells can also spill into the blood stream and spread the cancer around the body, including to other lymph nodes.
Hodgkin lymphoma tends to affect the lymph nodes in the head and neck whereas non-Hodgkin lymphoma can affect any lymph node or related tissue in the body.
Hodgkin lymphoma
Hodgkin lymphoma is distinguished from other types of lymphoma by the type of cancer cell formed – the Reed-Sternberg cell – which is not found in any other blood cancer.
The exact cause of this type of cancer is unknown. However, there is increasing evidence that infections (such as the virus that causes glandular fever) may play a part in its development, especially when it occurs in children.
Hodgkin Lymphoma has been reported to occur more frequently among young children from developing countries than among those from countries of advanced socio-economic status. There is an increased risk of the disease among parents, siblings and identical twins of lymphoma patients.
Incidence
Hodgkin lymphomas in children accounts for 45% of all childhood lymphoma diagnoses – around 60 children a year in the UK.
The disease predominantly affects older children, with two-thirds of cases occurring in the 10-14 year age group and no cases in infants.
Hodgkin lymphomas are almost twice as common among boys as among girls. This male excess becomes less marked with increasing age.
What are its symptoms?
Hodgkin lymphoma symptoms include a persistent (lasting a few weeks) painless swelling of a single lymph gland, usually in the neck, armpit or groin.
Cough or breathlessness can occur if the glands in the chest are affected.
Also fevers, sweats, itching and weight loss can occur.
The exact diagnosis will be confirmed by removing part or all of an affected lymph gland so that the cells can be examined in the laboratory. This is known as a biopsy and is usually carried out under general anaesthetic.
Further tests, such as X-rays, CT and MRI scans and blood tests are carried out to determine the exact size and position of the lymphoma and whether it has spread. This is known as staging.
Hodgkin lymphoma may be defined as stage 1, 2, 3 or 4, followed by A or B.
Stage 1 means that only one area of lymph nodes is affected at one site (either above or below the diaphragm – the muscle that separates the chest cavity from the abdominal cavity).
Stage 2 indicates that two or more areas are affected but, again, either above or below the diaphragm only.
Stage 3 implies lymph nodes are affected above AND below the diaphragm and possibly the spleen as well.
Stage 4 Stage 4 Hodgkin Lymphoma is the worst stage as it means the cancer has spread (to the liver, lungs or bone marrow).
A or B is added to the number to indicate whether there are systemic Hodgkin lymphoma symptoms (fevers, weight loss, night sweats). A is used when there are none of these symptoms. B means the symptoms are present and this implies the child is more unwell and needs more treatment.
You can learn more about lymphomas, including Hodgkin lymphoma with this informative video:
How is it treated?
The main treatment for Hodgkin lymphoma in children is chemotherapy. Sometimes radiotherapy is also required. If the cancer has not spread beyond its original site, radiotherapy alone may be used, following surgery to remove the affected lymph nodes. The type and amount of treatment given depends on the stage of the disease at diagnosis.
Where chemotherapy is used, it will usually be given every few weeks for a number of months.
Where radiotherapy is used, it is usually given for a few minutes each day over a period of two to four weeks.
Treatment may last for anything between a few months and two years, depending on the exact type of lymphoma and the stage to which it has progressed.
What are the side effects of Hodgkin Lymphoma treatment?
Treatment for Hodgkin Lymphoma often causes side effects. These will depend on the particular treatment being used and the part of the body being treated but may include:
- Hair loss
- Tiredness
- Nausea
- Vomiting
- Reduced resistance to infection
- Bruising and bleeding
- Diarrhoea
A small number of children may develop late side effects, sometimes many years later, that are caused by their treatment for lymphoma.
The main risks arise from the use of radiotherapy, which may impair growth and cause infertility. The risk of infertility is greater among boys and the risk is increased if both radiotherapy and chemotherapy are used.
There is a risk of hypothyroidism associated with irradiation to the neck.
Both radiotherapy and chemotherapy have been associated with heart and lung complications.
There is an increased risk of second cancers in those who survive childhood cancer, thought to be associated with the treatments used.
The possible risks of any treatment given will be explained by the child’s doctor before treatment begins. Every effort will be made to minimise the risk of these kinds of complications.
Follow-up
Children will have regular follow-up appointments, following their treatment. These appointments are to check for any recurrence of the cancer and for any problems that may arise as a result of the treatment they were given (late effects).
Occasionally, the cancer can recur. When this happens it is called a relapse. Relapse occurs most likely as a result of a few of the original cancer cells surviving the treatment. Sometimes, this is because cancer cells spread to other parts of the body and were too small to be detected during the follow-up immediately after treatment. Treatment of the relapse will vary and be discussed as it may differ from the original course of treatment.
Survival Rate
The survival rate for Hodgkin lymphoma is 90%. Almost all children with this cancer can be cured. It is important to note that survival rates vary depending on the stage of Hodgkin lymphoma.
Research
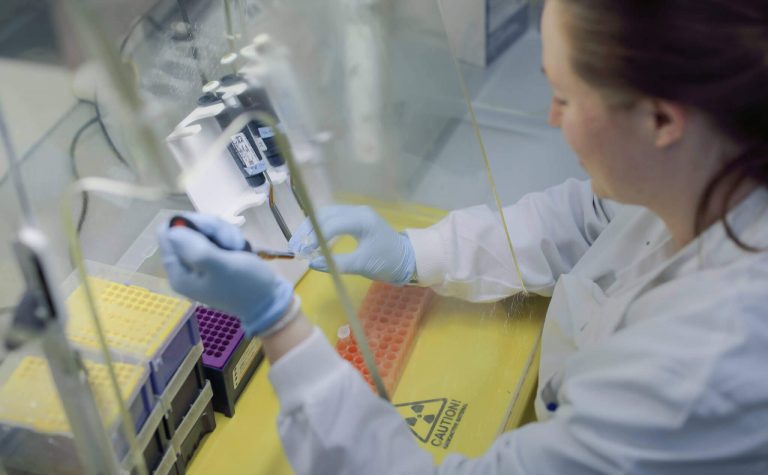
Many children have their treatment as part of a clinical trial.
Trials aim to improve our understanding of the best way to treat the cancer, usually by comparing the standard treatment with a new or modified version.
If appropriate, the child’s medical team will discuss participation in a relevant trial. Participation is optional but may offer the opportunity to receive new treatments.
Courtenay's Story
Courtenay’s victory against Hodgkin Lymphoma
 I was 13 when I was diagnosed with Hodgkin Lymphoma. My dad was the first to notice the lump on my neck. The left side had swollen to about twice the size of the right. That was Easter Sunday, 2001. Two days later, I was at the local doctor’s surgery being told I had glandular fever.
I was 13 when I was diagnosed with Hodgkin Lymphoma. My dad was the first to notice the lump on my neck. The left side had swollen to about twice the size of the right. That was Easter Sunday, 2001. Two days later, I was at the local doctor’s surgery being told I had glandular fever.
A blood test was taken, but it came back negative and I was sent for a biopsy. But even then the initial results were inconclusive. I was told I had something called toxoplasmosis; I just had to rest and I’d get better.
Two weeks later I had a different diagnosis: Hodgkin lymphoma. I’d always been a happy, healthy and active child. I was rarely unwell; I never missed school. Suddenly I was faced with six months of chemotherapy.
It got so hard to take the tablets that I was prescribed another tablet aimed at calming and relaxing me so that my throat would open up enough to swallow the other 16. But the treatment finally ended on November 30, 2001.
My mum and I both signed up to run the London Marathon for Children with Cancer UK, training through the wet and dark winter and doing our best to raise as much money as possible for the charity. As I crossed the line, my eyes filled with tears. Almost thirteen years after being diagnosed with cancer I’d run a marathon!
If you’ve been touched by Courtenay’s journey, help us invest in the high quality research that really matters which would otherwise go unfunded. This helps to support children with cancer so they can be with their families for longer.