About the research team
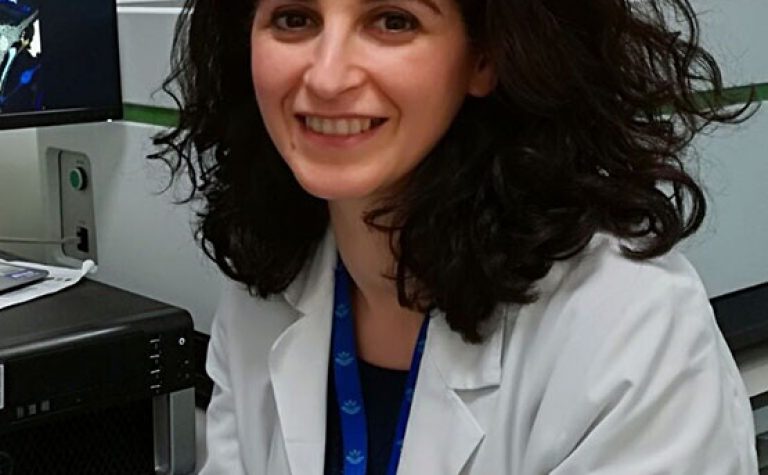
This project involves a collaboration between the Paediatric Endocrine Team at Great Ormond Street Hospital (GOSH) and the Developmental Imaging and Biophysics Section (DIBS) at the UCL GOS Institute of Child Health (ICH). The Neuroendocrine Division at GOSH cares for the largest single-centre cohort of children with Hypothalamo-Pituitary disorders in the UK. The Chemical Pathology Laboratory at GOSH is fully equipped to perform Enzyme-Linked Immunosorbent Assay (ELISA) and has already hosted a clinical PhD student for the development of biochemical assays for the measurement of hypothalamic peptides. The DIBS at ICH has access to advanced MRI facilities and expertise. The GOSH Neuroradiology Team has experience of interpreting brain images of complex and rare paediatric diseases. The key members of this project are Dr Manuela Cerbone, Prof Mehul Dattani, Dr Helen Spoudeas and Prof Christopher Clark. Dr Cerbone will have a pivotal role in the development/planning of the protocol, patient recruitment and data collection/analysis. She will be collaborating with various professionals in the DIBS ICH and GOSH Neuroradiology Departments for image analysis, and with clinical laboratory scientists and a previous PhD Student at GOSH for the hypothalamic peptides measurement. They will be linking with external laboratories (Newcastle, Manchester and Cambridge) for some of these hormone analyses. Prof Mehul Dattani and Dr Helen Spoudeas are the GOSH lead clinicians for congenital neuroendocrine disorders and for the late endocrine effects of childhood brain tumours, respectively. They have active research programmes in these fields. Prof Christopher Clark has a longstanding research interest on the application of novel neuroimaging methods for the understanding of neurological disability.