Sibylle and her team have dedicated the last 3 and a half years to their study, and have made an exciting breakthrough with osteosarcoma, the most common form of bone cancer in children, that affects approximately 30 children and their families in the UK every year.
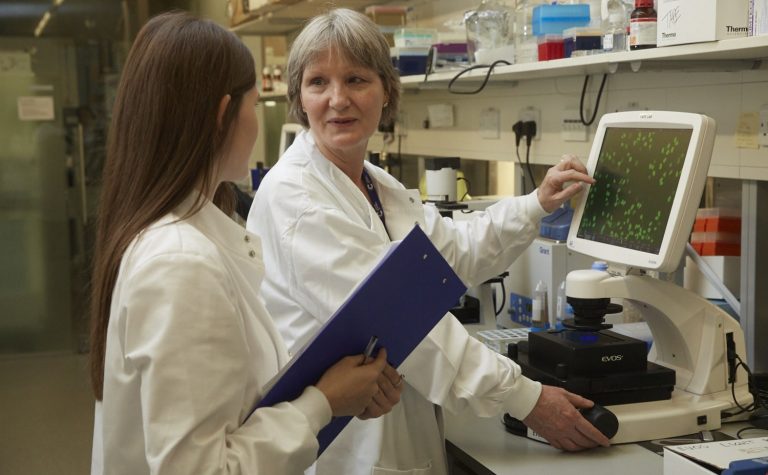
We caught up with Sibylle to find out more about her work, and what her research hopes are for the future. She writes:
Q: Can you tell us about your recent research?
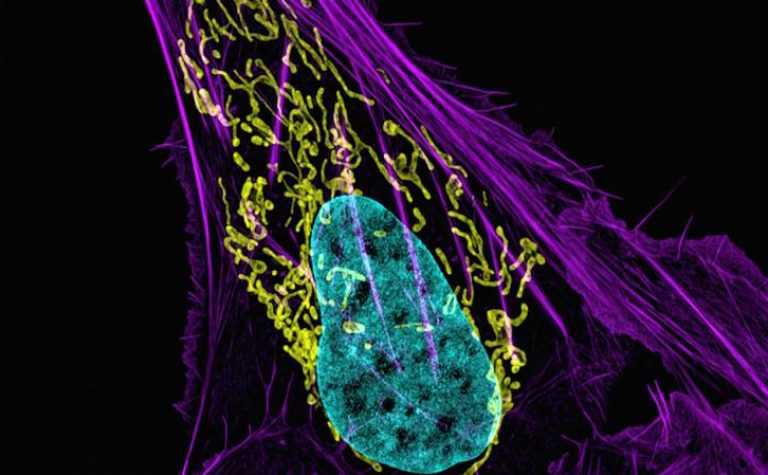
Our research provides evidence that a group of osteosarcoma (bone cancer) patients may respond to molecularly targeted anti-cancer drugs, called PARP inhibitors. These are currently used with notable success in adult patients with ovarian cancer. PARP (poly-ADP ribose polymerase) is a protein found in cells, and it helps damaged cells to repair themselves, therefore inhibitors stop repair that is specifically needed in certain cancers, for them to survive.
The PARP inhibitor drugs have very few side effects, and can be taken over a long period as a so-called “maintenance treatment”. Because of this, they can likely kill dormant (“sleeping”) cancer cells that may have migrated to other parts of the body once these regain division activity and then cause disease to re-occur.
We believe that replicating the treatment strategy already used in ovarian cancer in osteosarcoma patients may prevent deadly disease relapse that currently cannot be treated or prevented.
Q: Why is it so important to find new treatments for Osteosarcoma?
It is indisputable that a seismic improvement for osteosarcoma patients has come from high-dose chemotherapy, which has increased survival from less than 30% to near 70%.
However, one in three young osteosarcoma patients still die from cancer despite current treatment, and a solution must be found for them.
Importantly, patients, even if they do survive, pay a high price for the potential benefit of the current high dose chemotherapy regimen, often resulting in poor quality of life during treatment because of debilitating side-effects, and secondly a high incidence of long term damage in different organs.
It is these two problems that identify a clear need for more, and different, treatment options in addition to what we currently have! It is important to find alternative treatments that are effective, but kinder than our current treatment options.
One in three young osteosarcoma patients still die from cancer despite current treatment, and a solution must be found for them.