About the Research Team
Professor Cristina Lo Celso, is a scientist who works on leukaemia at Imperial College London. She has developed an amazing technique, using a powerful microscope, which enables visualisation of the interaction between fluorescently labelled leukaemia cells and other supporting cells in the bone marrow of live mice under anaesthesia. Dr Richard Burt (Imperial College London) works both as a doctor treating young adults with ALL and as a scientist investigating causes of treatment resistance in ALL. This grant would enable Dr Burt to establish his own lab focused on overcoming treatment resistance in ALL. Professor Rachael Hough (University College London Hospitals) is a doctor with several decades experience treating adolescents with ALL and has experience treating patients with Inotuzumab Ozogamicin.
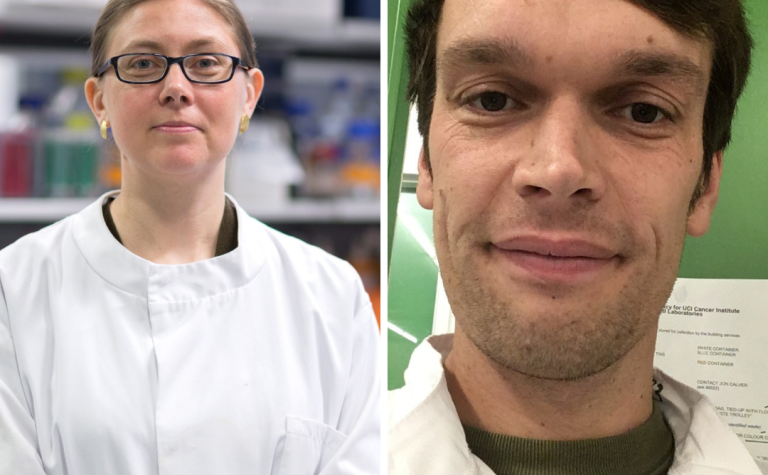
Dr Mariia Yuneva (Francis Crick Institute) is an expert on cancer metabolism and has developed several techniques to determine how the metabolism of cancer cells is altered to survive after treatment. Dr Samantha Atkinson (Imperial College London, Francis Crick Institute) is a very talented research technician, who has spent the past year learning techniques important for the project in Professor Lo Celso’s and Dr Yuneva’s labs. Sarah Jordan (University College London Hospitals) is a specialist young adult leukaemia nurse with many years’ experience and will aid in disseminating the research findings to patients and their families.