Meet the
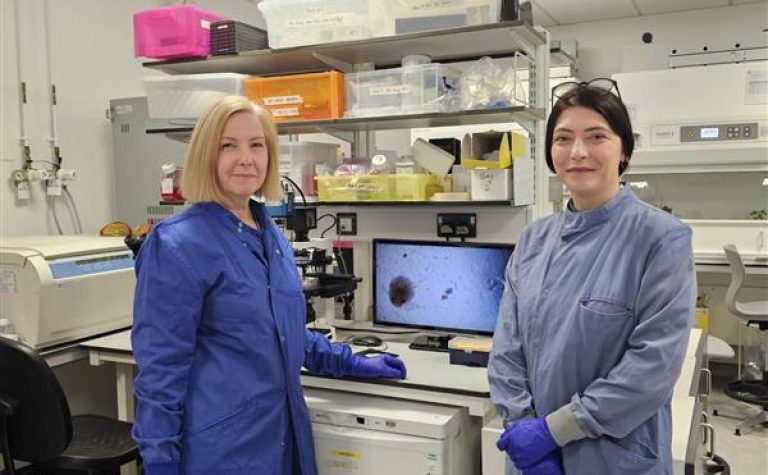
Brain tumour biology is hugely complex and understanding this requires a team of researchers with expertise in different areas. Dr Beth Coyle and her research team bring together expertise to work towards the shared goal of improving outcomes for children and young people with brain tumours.
Beth has been at the forefront of children’s brain tumour research in the UK for more than 20 years. She is a long-term member of the Nottingham Children’s Brain Tumour Research Centre which allows clinical and scientific researchers to pool their expertise towards better understand and treatment.
The research will take place in the University of Nottingham’s Biodiscovery Institute, a state of the art multidisciplinary research facility where the majority of the applicants are co-located.
Joining Dr Coyle’s team for this project are experts in generating the matrices needed to study 3D tumour growth accurately (Professor Alvaro Mata, School of Pharmacy), in studying the interaction of tumours with the immune system (Dr Andrew Jackson and Dr Judith Ramage, both School of Medicine), hypoxia (Dr Alan McIntyre, School of Medicine) and in understanding how drugs target cellular pathways in tumours (Dr Ian Kerr, School of Life Sciences and Dr Louise Fets, MRC London Institute of Medical Sciences).
The team is completed by a paediatric oncology clinician (Dr Tim Ritzmann, University of Nottingham/ Nottingham University Hospitals NHS Trust) and a neuropathologist (Mr Simon Paine, Nottingham University Hospitals NHS Trust) whose expertise at the interface between the clinical bedside and the laboratory bench will contribute greatly to ensuring the models we make are excellent mimics of the patient’s brain tumour.