Newsletter Signup x
Press release: 24th November 2017
“Taking into account key genetic abnormalities that influence outcome will ensure that MRD thresholds for more or less intensive chemotherapy are more flexible and each child gets the most appropriate treatment.
“The idea of combining or integrating MRD and genetic information to refine the allocation of patients to different risk groups has been fully adopted in the next clinical trial, which is currently being designed and will hopefully begin in late 2018.
“Risk stratification is a key component of improving survival rates and reducing side-effects for children with leukaemia.”
Cliff O’Gorman, Chief Executive of Children with Cancer UK, said: “By developing a new way of interpreting MRD, we can significantly improve the accuracy of predicting how likely it is that a child with leukaemia will relapse. This has made more personalised treatment a possibility for young patients since we launched the trial in 2003, and helped to drive five-year survival for childhood acute lymphoblastic leukaemia above 90%.”
“But there is still much more to do. Children and young people diagnosed with cancer face aggressive treatments that can have a long-term impact on their health and well-being. It is crucial that we build on this breakthrough and continue to fund further studies and clinical trials to develop kinder, more effective treatment for young cancer patients in the UK.”
Dr Alasdair Rankin, Director of Research at Bloodwise, said: “Current treatments for children with leukaemia are highly toxic and can have devastating side effects both in the short and the long term. New ways to reduce treatment intensity, without reducing chances of survival, are desperately needed. This study represents another advance in personalising care and should mean that more children get the right treatment for them.”
Dr David O’Connor, Consultant Paediatrician in Haematology at Great Ormond Street Hospital, said: “Through this new research we have been able to take an important step forward to identify, earlier on, leukaemia patients who require more targeted therapy. This study suggests that early detection of patients’ specific treatment needs can improve patient outcomes, and reduce the risk of relapse and complications for those patients identified. This study represents an exciting advance in personalised medicine.”
The researchers divided children into groups depending on whether their leukaemia cells contained genetic abnormalities known to be associated with a ‘good’, ‘intermediate’ or ‘high risk’ of relapse. While children’s genetic risk of relapse broadly corresponded with their MRD test – assigned risk category, this was not always the case.
The study found that children who had a ‘good risk’ genetic profile but whose blood was made up of between 0.01 and 0.1% leukaemia cells – just above the MRD threshold – actually had excellent chances of survival whether they were given standard treatment or intensive treatment. As a result of the findings, the MRD threshold at which children who are cytogenetic ‘good risk’ are treated with the most intensive treatment has now been raised, reducing treatment toxicity for around 50 children a year in the UK, without compromising their chances of survival.
The study also identified a group of children currently treated with low intensity chemotherapy as a result of their low MRD test results who also have high risk genetics and who experience high rates of relapse. Indeed, nearly all children in the high risk genetics group who did not have a negative MRD result a month after treatment had very high relapse rates and may respond better to new types of treatment.
By examining children’s MRD test results on a sliding scale, instead of whether they were simply above or below a certain threshold, the large-scale study demonstrated that children with very high levels of MRD treated with intensive treatment were much more likely to relapse than children who were just above the threshold.
ENDS
For further information please contact Hamir Patel hamir.patel@instinctif.com or telephone 07771 780 946
NOTES TO EDITORS
The report is published online in the Journal of Clinical Oncology under the title, ‘Genotype‐specific MRD interpretation improves stratification in paediatric acute lymphoblastic leukaemia’. Corresponding author: Prof Anthony V Moorman, Leukaemia Research Cytogenetics Group, Northern Institute for Cancer Research, Newcastle University, UK
About childhood acute lymphoblastic leukaemia (ALL)
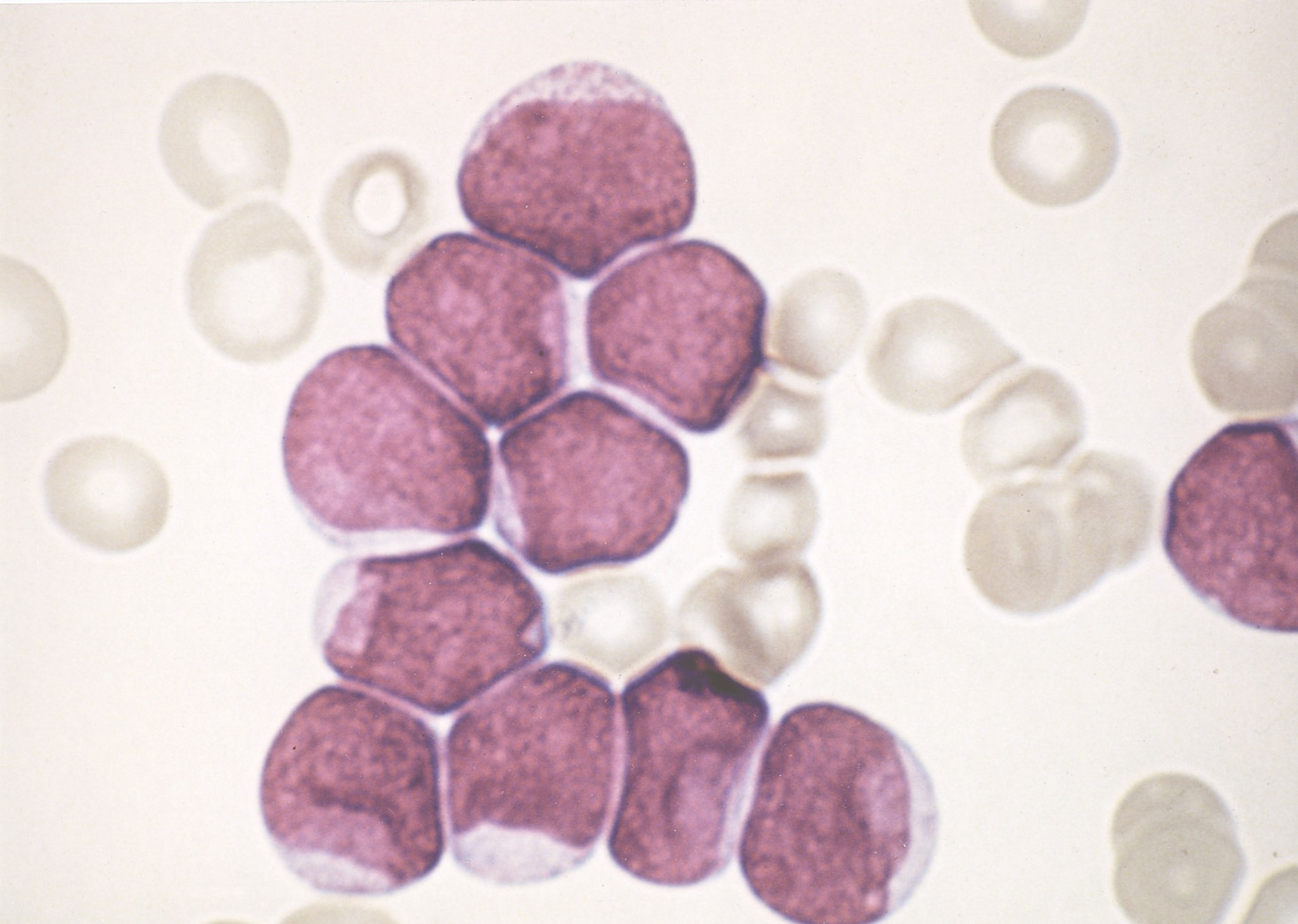
Leukaemia is the most common form of childhood cancer. It occurs when healthy white blood cells in the bone marrow develop DNA faults early in their development. These abnormal cells then multiply uncontrollably and live for longer than they should, crowding out normal blood cells. Acute lymphoblastic leukaemia (ALL), which starts in white blood cells called lymphocytes, is the most common form of childhood leukaemia and is diagnosed in around 400 children each year.
Symptoms vary from child to child, but common signs include tiredness, breathlessness, frequent infections, fever, bone pain or unexplained bruising. Treatment for ALL normally consists of a combination of different chemotherapy drugs and can last up to three years.
About Children with Cancer UK
Children with Cancer UK is the leading national children’s charity dedicated to research into cancer in children and young people. Inaugurated in 1988 by Diana, Princess of Wales, in memory of Jean and Paul O’Gorman our aim is to improve survival rates and quality of survival in young cancer patients and to help research ways of reducing cancer incidence. Every year we invest more than £4 million in new research across the full range of childhood cancers. We currently have more than 60 projects under way at leading centres around the UK.
About Bloodwise
Bloodwise is the UK’s specialist blood cancer research charity dedicated to improving the lives of people living with and beyond blood cancer. The charity, which was formed in 1960, changed its name from Leukaemia & Lymphoma Research in September 2015.
Around 39,000 people of all ages, from children to adults, are diagnosed with blood cancers and related disorders every year in the UK. It is a complex disease area made up of over 100 individual diseases. Some affect thousands of people, such as common forms of leukaemia, lymphoma and myeloma. Others affect only a handful. But together, blood cancers are the fifth most common form of cancer and the third largest cause of cancer death in the UK.
The charity’s research is targeted at understanding more about blood cancer, finding causes, improving diagnosis and treatments, and running ground-breaking clinical trials for patients. The charity champions patients’ needs by influencing relevant decision makers and influencers, and seeking to raise awareness of the issues faced by patients. Their patient services provide information, support and assistance to patients at every stage of their journey. For more information visit www.bloodwise.org.uk
Newcastle University, UK, is a thriving international community of some 27,750 students from over 130 countries worldwide.
As a member of the Russell Group of research intensive universities in the UK, Newcastle has a world-class reputation for research excellence in the fields of medicine, science and engineering, social sciences and the humanities.
Its academics are sharply focused on responding to the major challenges facing society today. Our research and teaching are world-leading in areas as diverse as health, culture, technology and the environment.
The Research Excellence Framework 2014 (REF) placed Newcastle University 16th in the UK for Research Power and the vast majority of our research (78%) was assessed to be world-leading or internationally excellent.
Newcastle University is committed to providing our students with excellent, research-led teaching delivered by dedicated and passionate teachers. This is reaffirmed by achieving the best possible outcome – a Gold Award – in the Teaching Excellence Framework (TEF). Based on the evidence available, this means that the TEF Panel judged that Newcastle University delivers consistently outstanding teaching, learning and outcomes for its students of the highest quality found in the UK.
About Great Ormond Street Hospital for Children NHS Foundation Trust
Great Ormond Street Hospital is one of the world’s leading children’s hospitals with the broadest range of dedicated, children’s healthcare specialists under one roof in the UK. The hospital’s pioneering research and treatment gives hope to children from across the UK with the rarest, most complex and often life-threatening conditions. Our patients and families are central to everything we do – from the moment they come through the door and for as long as they need us.